
The book is also helpful to students engaged in their internal medicine and surgery clerkships, and to house officers as an up-to-date summary of relevant physiology and a source of key references. It is valuable to students early in their medical school years by highlighting the clinical relevance of their basic science courses, and in preparation for their USMLE Step 1 examinations.

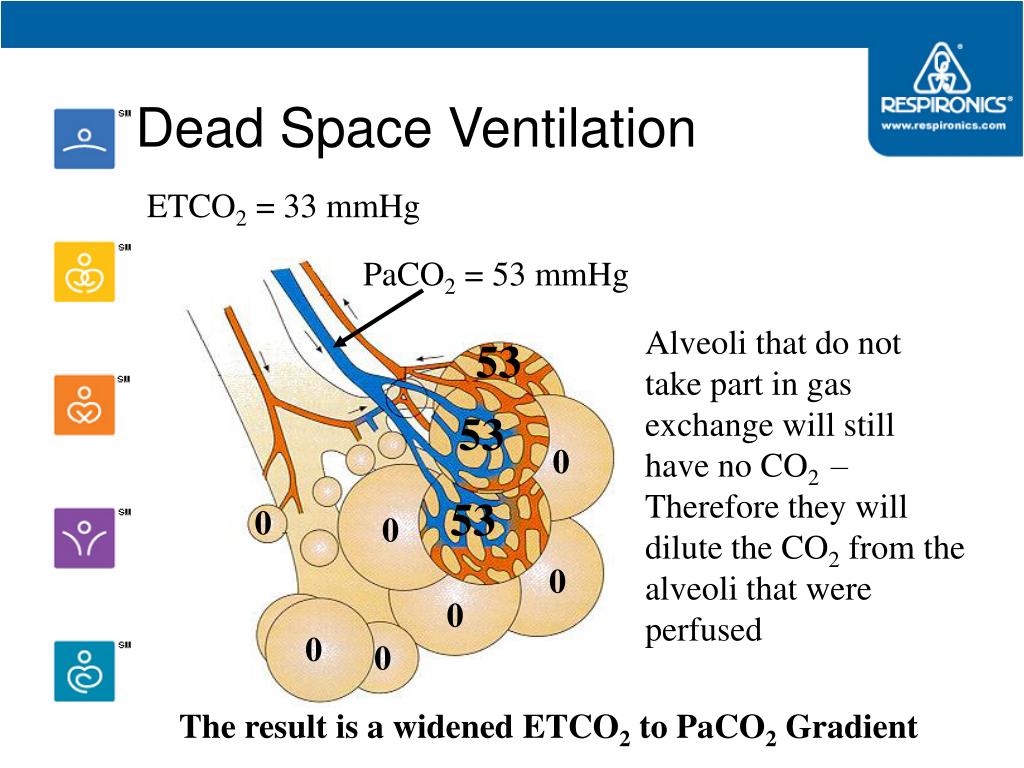
The A-a gradient can be calculated by subtracting the alveolar partial pressure of oxygen, which is calculated using the alveolar gas equation, by the arterial partial pressure of oxygen, measured with arterial blood gas (ABG).The book has proved useful as a text for both Pathophysiology and Introduction to Clinical Medicine courses in medical schools, and it has been popular in similar courses in nursing schools, physician assistants' training programs, and other allied health programs. All three of these conditions can contribute to an increase in A-a gradient and cause hypoxemia. Diffusion problems can occur when the alveolar walls are fibrosed and oxygen cannot diffuse across the alveolar wall into the blood stream. High V/Q is also called dead space and low V/Q is called shunting. V/Q mismatch means a mismatch of ventilation to perfusion (V/Q) ratio and can represent either too little perfusion due to blood flow obstruction (high V/Q) or too little ventilation due to airway obstruction (low V/Q). An increase in A-a gradient can occur in hypoxemia and the causes include V/Q mismatch such as dead space or shunting and diffusion problems. The normal A-a gradient is 10 to 15 mmHg. The A-a gradient represents the difference in partial pressure of oxygen between the alveoli and the arteries.


 0 kommentar(er)
0 kommentar(er)
